Dr. Zema received his Medical Degree from Cornell University Medical College and completed his post-graduate Internal Medicine training at the North Shore University Hospital in Manhasset, Long Island, with subsequent Fellowships in Cardiology at that institution and The New York Hospital Cornell Medical Center in Manhattan, NY. He is a distinguished Fellow in the American College of Physicians, American College of Cardiology, American College of Chest Physicians and the American College of Clinical Pharmacology among others, and is a Certified Physician Executive of the American Association of Physician Leadership and a Six Sigma Green Belt in Healthcare. Dr. Zema has penned numerous publications in professional medical journals and most recently has authored the book “Modern Healthcare Delivery, Deliverance or Debacle – A Glimpse From the Inside Out.”
FMM: Take us back to your time working at Brookhaven Memorial Hospital Medical Center in NY.
After finishing my Cardiology specialty training at the New York Hospital and its Cornell affiliate, North Shore University Hospital (NSUH), like others you essentially have three choices: stay at the university training center in some capacity if offered the opportunity, apply for a similar position at another academic institution or put out a shingle and open a Cardiology practice. I became aware that a community hospital on Long Island NY, about 40 miles east of where I was finishing up my training, might have a need for a Cardiologist. I was interested in clinical research, however, and as such was encouraged by the Chairman of Medicine at NSUH to stay on there. Actually, I was warned, “You can stay on here and participate in clinical research or take that other opportunity at the community hospital out east and do private practice – but you can’t do both – it’s research or practice.” After having arranged the appropriate out-of-town interviews, I was even more shocked to learn that individuals in that community, only 60 miles from downtown Manhattan, had often been forced to travel westward to the next county, merely to get a stress test or have an echocardiogram performed! I promised the Board of Directors there that I would change that and within a month or two had signed a contract with Brookhaven Memorial Hospital Medical Center in Patchogue, Long Island – a 306 bed institution serving more than 400,000 people in 28 different communities.
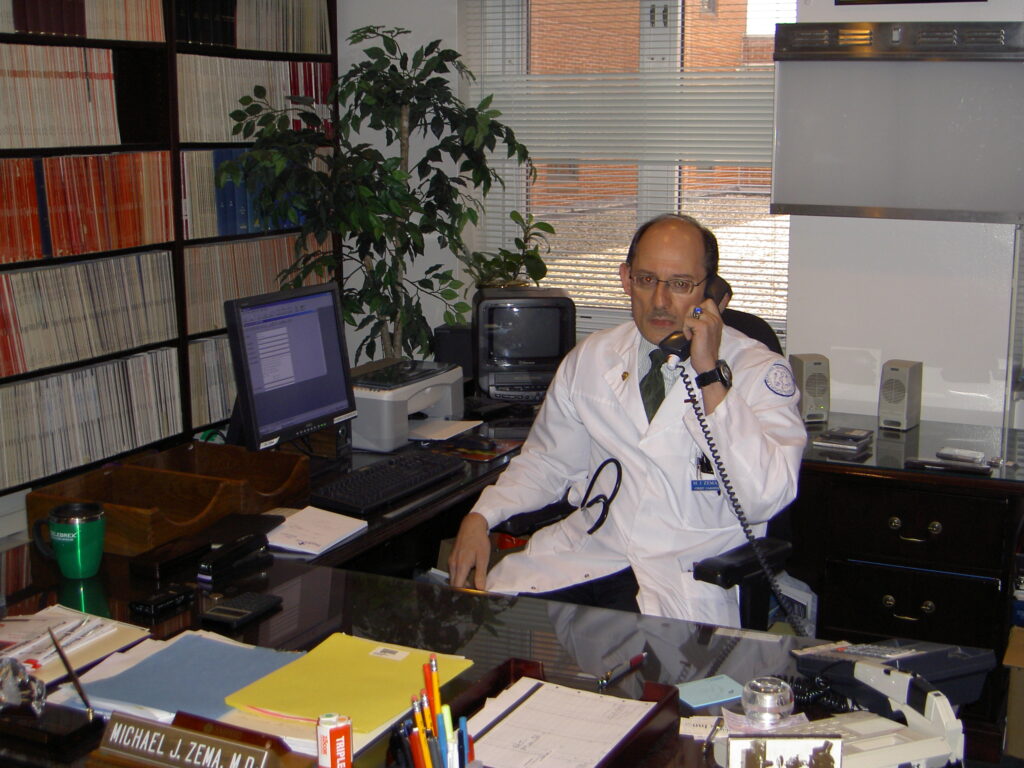
A month later, I rented an apartment in the area and started working. I was appointed “Director of Cardiology,” a salaried position in a department of one – me. For my office, I was given a converted equipment storage closet on the 4th floor of the hospital, which was furnished with a not so comfortable metal folding chair and a small metal folding table upon which a used IBM Selectric typewriter had been placed, so I could type my own patient consultation notes. For a patient examination table, I was offered the use of the hospital’s 4th floor “treatment room” down the hallway from my “office” if it was available. This was roughing it! With four years of medical school, three years of post-graduate medical residency and two additional years of cardiology fellowship training, what had I gotten myself into? By the next year, however, having demonstrated hard work on my part, the hospital had created my own small office with its own examination room, had purchased cardiac ultrasound and stress testing equipment and the Cardiology Department had grown to three individuals, myself, an RN and a departmental secretary. Life was not good, but was starting to get better. Fast forward 26 years and with grass roots fund raising, and a commitment on behalf of myself and multiple hospital Boards of Directors, my department had grown to over 35 employees including clerical, nursing, technologists, and exercise physiologists performing annually over 5,000 non-invasive cardiology tests, offering full cardiac rehabilitation services, having a secured certificate of need for a cardiac catheterization laboratory, and having added seven additional practicing cardiologists consistent with the old adage – “if you build it, they will come.” And lo and behold, I had a spacious, beautifully designed and furnished office with my own dedicated administrative assistant. And despite that ominous warning from my previous Chairman of Medicine at NSUH, I had also succeeded in publishing over 80 scientific research papers and abstracts solely while based at this community hospital with no formal academic ties. While at Brookhaven, I had the opportunity to become a permanent member of the Hospital’s Medical Board, Vice President of a Physician Independent Practice Association and Board Member of a Physician Holding Company, allowing me to draw upon those experiences years later when sitting down to write my book.
FMM: So, where did life take you after leaving Brookhaven Memorial Hospital?
After twenty-seven years at the helm in cardiology at Brookhaven, all parties, myself included felt that perhaps it was time for a change. I was proud of what I had built – a well respected, thriving Cardiology Department within a community hospital which through my clinical research efforts had also attained a certain level of prestige, locally, regionally and even to a limited extent nationally. Over the years, I had also personally provided cardiology services to over three thousand patients that having learned of my imminent departure, would now need to have their follow-up care arranged. While I could have “sold” my practice to a number of the cardiologists practicing at the Hospital, I elected instead to “give” my patients’ medical records to Dr. Satheesh Joseph, a young man finishing up his cardiology fellowship training program at the State University of New York whom I had previously mentored in the field of nuclear cardiology. He was bright, energetic, with a young family, living on a fellowship training stipend, whom I felt could well use a “running start” in what at the time locally was a rapidly tightening physician market place. Some years later, in gratitude, he was to invite me back to Long Island to perform the ribbon cutting at the opening of his new cardiology facility, “Brookhaven Heart.”

Dr. Jospeh opening for Brookhaven Heart
Looking for a change in scenery, for the next few years, I worked as a clinical cardiologist for Kaiser Permanente in Moanalua, Hawaii on the Island of Oahu. There I had my first intense exposure to the EPIC electronic medical record, as Kaiser was far ahead of hospitals in New York at the time in the application of that technology. This experience again would serve me well years later when preparing my book manuscript. Renting a high rise apartment one block from the beach at Waikiki, and working out at the local gym on Kalakaua Avenue while watching the surfers ride the waves, was certainly a change in scenery from Patchogue, Long Island and one which Mrs. Zema enjoyed immensely.
While in Hawaii, I had learned of an opportunity at the University of Tennessee (UT) Chattanooga. They were apparently interested in converting to a full time salaried staff model the cardiology service line at their flagship hospital, Erlanger Medical Center. Previously, cardiology physician services had been outsourced to a physician group primarily practicing at a competing institution. Apparently, the search committee must have been somewhat impressed by what I had created from scratch at the community hospital level on Long Island. An offer was made and I accepted the role of Professor of Medicine at UT Chattanooga and Chief of Cardiology at the Erlanger Health System, the 9th largest public hospital in the country. During my tenure there, I was instrumental in designing and staffing a large outpatient cardiology clinic, recruiting highly qualified subspecialists in cardiology and enhancing the cardiology teaching service for the existing Family Practice and Internal Medicine residency programs. This exposure and experience in formal academia would again serve me well years later at the time of book writing.
After leaving Erlanger, I elected to remain in Chattanooga, and for two years worked as a cardiology specialty physician reviewer for a large nationally recognized radiology benefits manager whose clients included over 90 different insurance companies. While I had interacted in the past with such reviewers as the patient provider and advocate myself, now I had the opportunity to sit on the other side of the desk and witness first hand some of the frustrations experienced by thousands of primary and specialty care providers seeking pre-authorization insurance approval for testing to be performed upon their patients – once again, more exposure and great fodder for my future book.
FMM: What has surprised you the most about the public’s perception of healthcare delivery and how did it lead you to write your book?
I was struck by the general community’s total naivete about a subject so fundamentally important to each and every one of us. The lack of knowledge and degree of misinformation that abounds in regard to healthcare delivery is simply astounding. Even among those involved in healthcare delivery, each operate in their own little “silo,” often oblivious to the workings taking place in the other “silos” around them, as well as the multiple interactions across these silos necessary to maintain the functionality of our rather complex healthcare delivery system. For those not directly involved in healthcare, their exposure to the system is often relatively brief, surely intermittent, and largely gleaned from the outside looking in. I wanted to write a book for those who dared to see what’s on the other side of the curtain — healthcare delivery seen from the inside looking out.
FMM: “With the inherent potential of Artificial Intelligence (AI) deliverance from the illnesses that have plagued mankind may finally be within reach.” Please explain.
Medical knowledge is growing exponentially. The bases for diseases, both genetic and acquired, previously unknown, are now being uncovered at rates thought impossible virtually only a few short years ago. I could argue that for a human brain to assimilate all this new medical knowledge, even in a single medical discipline, is an impossibility. Machines, however, do not suffer from man’s inherent limitations. Natural Language Processing (NLP), a subset of AI, allows machines to identify and interpret meaning from human language. NLP has already been increasingly used to extract useful information from unstructured data made available through electronic medical record systems for quality improvement and clinical research. Machine Learning (ML) and even more so Deep Learning (DL) computer software can actively learn outside the bounds of normal programming. A typical computer program uses an if-then statement mechanism or mentality, meaning there is an explicit code that directs the software to produce y when given x. However, ML is capable of processes that are not explicitly coded and is therefore able to dynamically learn from new information as it experiences it – assimilate it, bank it, and refine it by further assimilating new information, over and over without fatigue and at lightening speeds. Used properly, with the appropriate ethical safeguards in place, the possibilities of AI when applied to healthcare are boundless.
Your new book, “Modern Healthcare Delivery Deliverance or Debacle – A Glimpse From the Inside Out” focuses predominantly on changes to the healthcare delivery system in the past thirty years or so. Tell us about some of those BandAids, as you’ve called them in your book, that having been applied to the ailing healthcare delivery system have not only not met some of their goals, but also have had unintended consequences for patients and providers.
Among some of these BandAids, to name just a few, are the Managed Care HMO’s of the ‘90s, the Pay-for-Performance programs of the past vicennium, Accountable Care Organizations and the Electronic Medical or Health Record (EHR). Although I could cite many more, as most today own and operate a smartphone, tablet, laptop or some combination thereof, it’s probably easiest for me to use EHR as an example.
As information technology became less expensive, and the vulnerability of a paper record became clear after such natural disasters as Hurricane Katrina, the trend away from the paper medical record toward more widespread use of a digital electronic health record (EHR) was accelerated by federal legislation designed to speed its adoption. Physicians could now directly place their own patient orders into the EHR through a series of clicks, thereby avoiding the need for their handwriting to be deciphered by another, thus lessening the chance for medical errors. Providers could also be “nudged” in real-time by computer “decision support software” to alter or at least adjust their patients’ orders based upon resource availability or comparative cost analyses. Potential adverse medication interactions could be caught at the very instant the provider attempts to place the medication order. Needless duplication of testing can be prevented as the provider can be notified, again in real-time, that a similar or identical test has recently been performed by a different provider. Patients can have easy access to their personal medical records through the use of “patient portals.” So far, everything sounds great.
With EHR, however, comes an enhanced potential for breach-of-privacy of patients’ medical records. This vulnerability, moreover, is not confined to the individual practitioner’s office. Pernicious cyberattacks have already been successfully directed at the patient data base of entire healthcare systems. Should sensitive health information be available through the patient portal? For example, should the totality of a provider’s notes about a patient exhibiting signs of cognitive decline or frank dementia be accessible to the patient in the name of transparency? With the provider fixated on the computer screen at the time of a patient encounter, is there not a loss of doctor-to-patient communication? With various providers having seamless electronic access to patients’ medical records, is there not also a loss of personal doctor-to-doctor communication about a given case? By use of the copy and paste software command with its ability to populate the medical record with an immense amount of data, much of it unrelated to the patient’s current problem, “note bloat” is often created making it more difficult for others to actually find the needed nugget of information. As one physician once described it, “It’s like getting a big box full of packaging material, and there’s a thumb drive buried somewhere in it.”
FMM: What are some of the drivers of healthcare costs that stand in the way of attaining a healthcare delivery system that delivers high quality, is more equitable and still nevertheless remains fiscally sustainable? At this point in time, can the system be fixed?
“Waste,” as exemplified by the performance of needless services may be the final common pathway for a number of other drivers such as the practice of defensive medicine, and the potentially self-serving fee-for-service payment model. Having said that, however, interestingly studies across various populations have revealed that up to one-third of care provided has been either of equivocal value or inappropriate regardless of whether care had been provided in a single-payer or fee-for-service environment. Other heavyweights include the excessive administrative costs associated with a multi-payer system, and the various financial barriers to patient care, the latter ultimately trickling down to the lack of a fiscally and politically acceptable form of universal healthcare. For these and other drivers of healthcare costs, I offer potential solutions designed to maximize value without diminishing quality. Some of these might themselves be criticized as mere additional BandAids, albeit previously untried and in my opinion worthy of a trial, while others are more draconian in their reach. In my book for purposes of clarity, I discuss these separately but make the point that in reality many of these drivers are inexorably interlaced, and as such, any potential solution to one will have requisite effects upon the others.
For many of these drivers to be meaningfully mitigated, if not expunged, a change in behavior on the part of the physician or alternative provider is going to be necessary. Why, because these individuals are the gatekeepers of healthcare resources that ultimately result in downstream healthcare costs. While hospitals may provide the needed infrastructure and insurance companies and healthcare organizations the needed administrative support, it is the physician or alternate healthcare provider who serves as the gatekeeper for the patients’ entry into the healthcare system. Without the healthcare provider, there can be no healthcare delivery, no use of healthcare resources, no healthcare outcomes, and of course, no healthcare costs.
FMM: Where can we find your book?
You can find it at many of your favorite bookstores as well as for purchase in print or eBook versions online.